20 years ago today, my mum picked me up from my university dorm room and brought me to the ER where I was diagnosed with type 1 diabetes. I spent a couple of nights in the intensive care unit, then 3 days learning the basics of diabetes management. Then I was sent out into the real world to learn what it was really like to live day to day with my newfound life mate.
During the last 2 decades (or 240 months or 1044 weeks or 7305 days, but who’s counting?!), I have been:
• checking my blood glucose levels,
• injecting or infusing insulin,
• counting carbs,
• trouble shooting basal rates,
• treating lows,
• riding the blood sugar roller coaster,
• dealing with burnout,
• sticking medical devices on (and in) my skin,
• filling insulin pump reservoirs,
• scrambling to get sugar into my mouth,
• battling high glucose levels that won’t come down,
• being part robot,
• planning my meals,
• thinking like a pancreas,
• feeling overwhelmed at times,
• waiting for doctor and hospital appointments,
• trying not to feel judged by the number on my glucose meter,
• calculating insulin doses,
• reassuring my family – and myself,
• making sure I don’t run out of diabetes supplies,
• having my eyes, heart and feet checked,
• choosing my clothes carefully,
• sewing pockets to house diabetes devices,
• avoiding door knobs,
• lacking sleep,
• eating candy as medicine,
• toting around a ridiculously heavy hand bag to store all my diabetes crap,
• nursing bruises from injections and pump sites,
• dealing with discrimination,
• silencing the beeps,
• finding the right diabetes technology to fit my life,
• improving my math skills,
• wearing blue,
• sticking up for myself,
• participating in clinical trials,
• reading scientific papers,
• finding my tribe,
• being inspired by so many others living with diabetes,
• running a marathon,
• engaging in advocacy,
• volunteering for my local diabetes association,
• organizing diabetes peer support initiatives,
• using skills learned from living with diabetes in my professional life
• learning from other people’s stories,
• becoming an expert,
• sharing my experiences,
• teaching medical students about patient perspectives,
• attending and talking at medical conferences,
• kicking diabetes’ butt,
Oh, and also generally getting on with the rest of my life.
Sorry, that got a little out of hand, but once I started typing, the list kind of grabbed a life of its own. There is no question that diabetes is a full time job and this list only scratches the surface of the mental gymnastics that living with D involves. I guess the point is that diabetes has added a lot to my life, some of it downright horrible, some of it tedious and time consuming, some of it stressful and emotionally difficult, and some of it utterly amazing. I could not have gotten this far without the ongoing support I have from my family and friends and of course, the amazing people with diabetes I have met along the way, in person or in the DOC.
And as a little diaversary gift, my diabetes gave me this today:
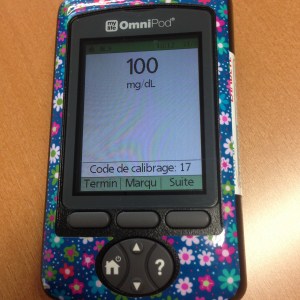
It doesn’t happen all the time, so it’s worth celebrating !